Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
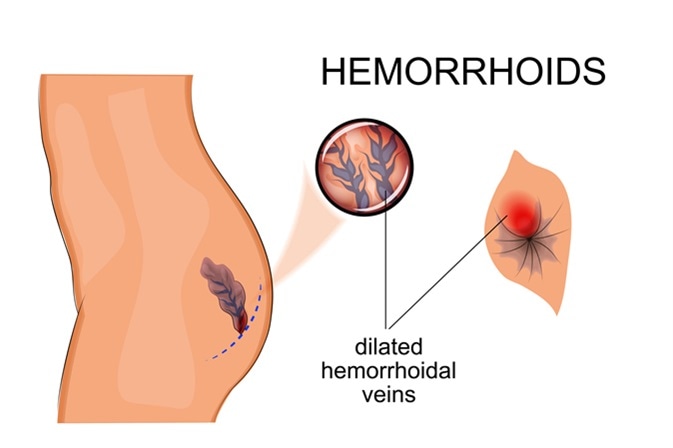
Also referred to as haemorrhoids, piles are swollen veins inside the anal canal (internal heamorrhoids) or around the anus (external haemorrhoids). When anal or rectal tissue that has become swollen gets damaged, bleeding and pain may result.
Often, piles are not associated with any symptoms and people are not even aware that they have them. If symptoms do develop, they may include:
Piles often clear up by themselves, although dietary changes and simple treatments may be recommended to relieve symptoms in the meantime. Severe piles may require more intensive treatment, which will depend on their location.
Non-surgical treatments to treat piles located in the upper two thirds of the anal canal may include:
However, piles located in the lower third, closest to the anus, will require surgery under anesthetic, since the amount of pain-sensing nerves in this area would mean the use of non-surgical techniques would be too painful.
Although piles can usually be treated using lifestyle changes, creams, ointments or non-surgical techniques, around one in ten individuals will require surgery. The main surgical procedures that are used to treat piles are haemorrhoidectomy, stapling and haemorrhoidal artery ligation.
Haemorrhoidectomy refers to the surgical removal of internal or external haemorrhoids, usually while a patient is under general anesthetic. This is the most effective method for treating severe haemorrhoids.
Closed haemorrhoidectomy is the most commonly used surgery for internal haemorrhoids. Haemorrhoids are excised using a sharp instrument or laser and the wounds then closed by suture. Following the procedure, patients are advised to take sitz baths, avoid becoming constipated and use mild painkillers. The procedure is successful in almost all cases, but potential complications include the following:
Closed haemorrhoidectomy is associated with the most post-operative pain, but it does provide the best results in the long term and is also associated with the lowest recurrence. Currently, researchers are trying to develop methods that can decrease the post-operative pain.
Open haemorrhoidectomy also involves excision of the hemorrhoids while a patient is under general anesthetic, but the wound made to remove the haemorrhoids is left open. This may be the preferred method when haemorrhoids that are extensive or awkwardly located, would make closing the incision difficult or increase infection risk after the procedure. The complications associated with this form of hemorrhoidectomy are similar to those associated with the closed procedure.
Also called stapled haemorrhoidopexy, this method is an alternative to haemorrhoidectomy and is also sometimes used for the treatment of prolapsed haemorrhoids. Stapling is less widely used than it was previously due to a slightly increased risk of serious complications, compared with other techniques.
The procedure involves stapling the last section of the large intestine, which decreases blood supply to the haemorrhoids and causes them to slowly shrink. It also lowers the likelihood of haemorrhoids prolapsing. Patient recovery time is faster than with haemorrhoidectomy and patients can usually return to work within a week of the procedure. It is also associated with less post-operative pain.
This procedure is a safe and effective alternative to haemorrhoidectomy and stapling. The aim is to limit blood supply to the haemorrhoids.
An ultrasound probe is placed inside the anus and used to locate the vessels that supply the haemorrhoid, which are then closed with a stitch to block blood flow. With its blood supply cut off, the haemorrhoid starts to shrink. Stitching can also be used to treat prolapsed haemorrhoids that are hanging from the anus.
Haemorrhoidal artery ligation causes less post-operative pain than the other procedures and patients report high levels of satisfaction with the results. The technique is also associated with a faster patient recovery time. There is a low risk of pain and bleeding during bowel movement, although this usually resolves within a few weeks.