Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
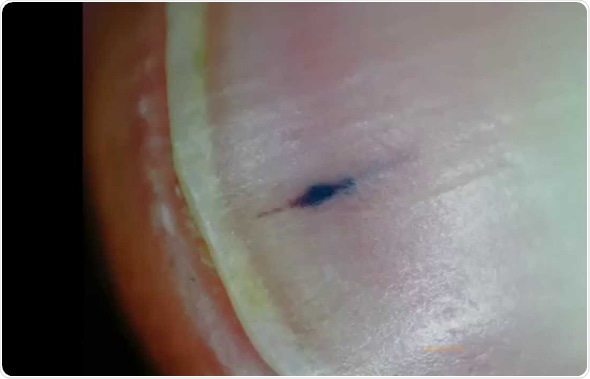
Splinter hemorrhages are essentially small spots of blood caused due to bleeding under the nails. The nail bed, or the skin under the tough surface of the nail, has a number of small blood capillaries running through it.
When they burst a tiny bleeding point comes up, which becomes visible through the nail plate. They are referred to as splinter hemorrhages as they are subungual, linear, dark streaks visible on the nail i.e., like splinters under the nail.
There is no physical pain or discomfort associated with the hemorrhages unless it has been caused by a physical trauma such as a bang to the fingernail. Usually they will grow out along with the nail and within three or four months the hemorrhage lines are no longer seen.
If they do not disappear and are formed without any injury to the fingernails, there may be another cause for the splinter hemorrhages. In case they begin to appear on more than one nail for no apparent reason, it would be a good idea to identify the cause.
Hemorrhaging can take place due to a physical injury to the nail bed, which the individual may have sustained. These bleeding points will usually vanish on their own as the effect of the physical trauma heals.
It takes a few months for the completely healthy nail to regrow. Sometimes splinter hemorrhages are seen on the nail when there is no history of physical injury. This may be a symptom for another underlying disorder.
The two most common causes of splinter hemorrhages are bacterial endocarditis and scleroderma. In bacterial endocarditis, an infection is present in the endocardium (the inner lining of the heart).
This happens when bacteria or other pathogens move from the mouth into the bloodstream and eventually reach the heart. It can cause damage to the heart valves and, if left unchecked, may even become life threatening.
Scleroderma is an autoimmune rheumatic disorder. Since the skin hardens in the disease, diagnosis may need both a rheumatologist and a dermatologist to conduct specialized tests.
As it is similar to other autoimmune diseases, diagnosis can be complicated. This chronic connective tissue disease can range from being life threatening to extremely mild depending on the organs it affects.
Other systemic causes for splinter hemorrhages may include rheumatoid arthritis, internal malignancy, mitral stenosis and systemic lupus erythematosus, antiphospholipid syndrome, peptic ulcer disease, malignancies, oral contraceptive use, pregnancy, and psoriasis.
This is an indicative, and not an exhaustive, list of conditions which may cause minor bleeding of the nail bed.
In some individuals the splinter hemorrhage lines show up without any known cause – such cases are called idiopathic.
In others, the individual may be already on some medication for another disorder and the drugs may predispose them to splinter hemorrhaging.
A qualified health care professional will need to make the actual diagnosis for the underlying cause.
Since the obvious physical injury is already known to the individual, it is the easiest to be diagnosed.
However for the other diseases there will be a battery of specialized tests that the individual will need to undergo to isolate the actual reason that splinter hemorrhaging is taking place.
These tests could include routine blood examination, blood cultures, complete blood count, erythrocyte sedimentation rates, x-rays of the chest region, electro cardiograms, echo cardiograms, etc. as prescribed by the attending health care professional.
The tests will hope to isolate the true disorder leading to splinter hemorrhages on the fingernails.
Resolution of splinter hemorrhage caused by physical trauma usually occurs without treatment within a couple of months. The body’s ability to regenerate itself is remarkable in such cases.
Provided there is no systemic disease, the splinter hemorrhages will disappear on their own. However if they have not disappeared after about three months, visiting a health care professional is recommended to identify the cause.
Once the investigative tests have revealed the underlying disorder responsible for the splinter hemorrhages, treatment will begin. As the underlying disorder is cured, the bleeding of the nail bed clears up automatically.
The treatment of bacterial endocarditis usually entails medication and possibly surgery to repair the heart valves if necessary.
There is no specific treatment for scleroderma, but various ways to manage it will be shared by the health care professional.
Topical ointments are usually prescribed to avoid secondary infections from setting in. As for the rest of the diseases which may cause splinter hemorrhaging, the treatment will be carried out as appropriate.
It is important to know that bleeding of the nail bed may also occur for no particular reason in some individuals. This does not automatically make it a symptom of a larger problem.