Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
Research finds a majority of people with rheumatoid arthritis (RA) are also vitamin D deficient and deficiency may worsen RA symptom severity. The most common causes of vitamin D deficiency in rheumatoid arthritis patients are insufficient intake of vitamin D from food sources, limited exposure to sunlight, and having a disorder that limits the body’s ability to absorb vitamin D in the body.
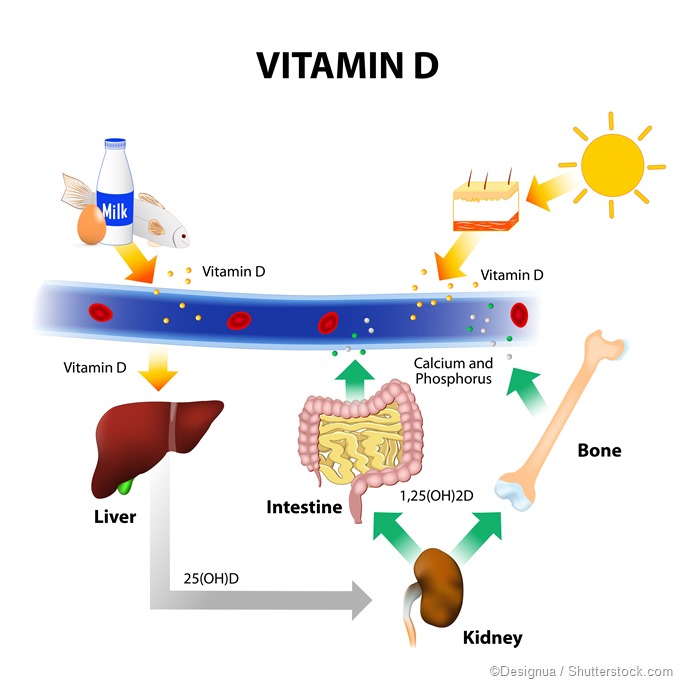
Vitamin D metabolism diagram.
Vitamin D deficiency has been strongly associated with disabling symptoms among those with rheumatoid arthritis, this according to a 2012 Greek study reported in Therapeutic Advances in Endocrinology and Metabolism. This is may be due to the fact that RA can affect the body’s ability to absorb vitamin D from the foods we take in, and when vitamin D levels are low, RA symptoms and pain may worsen.
Taking in more vitamin D - thrugh supplements and increased exposure to sunlight - can help to reduce inflammation, strengthen bone cartilage, and minimize pain and risk for disability. Vitamin D supplements can also help to alleviate other symptoms of arthritic conditions.
A 2004 study, with results published in Arthritis & Rheumatism, supports the idea that vitamin D plays an important role in preventing RA. The study looked at about 30,000 women between the ages of 55-69 years who did not have a history of RA.
After 11 years of follow-up with the women, including checking vitamin D levels, 152 cases of RA were confirmed. The researchers' findings were suggestive of an increased risk for RA in older women with lower vitamin D levels but researchers agreed the results were only preliminary.
Newer studies have disputed the claim that low vitamin D levels increase the risk for developing RA. A 2011 review in Seminars in Arthritis and Rheumatism looked at several studies examining the relationship between RA and vitamin D. The researchers reported they were not able to point to enough evidence to confirm low vitamin D is a risk factor for developing RA.
A study out of the Albert Einstein University of Medicine of Yeshiva University in New York City, found that people who take corticosteroid medications are twice as likely to become vitamin D deficient, compared to those who don’t take them.
Corticosteroid medications, such as prednisone, prescribed to reduce inflammation in RA patients, can reduce calcium absorption and impair vitamin D metabolism. Other RA medications, such as Hydroxychloroquine and immunosuppressants are also linked to malabsorption of vitamin D. If you are taking these medications to treat RA symptoms and pain, it is important to have your levels checked regularly.
These is also an increased risk for RA patients who are restricted from going outside due to mobility issues and disability, live in parts of the world where sunlight is limited during the winter months, have dark skin, or who frequently wear clothing covering most of the body.
Symptoms of vitamin D deficiency for patients with RA include worsening pain, depression, weak bones, fatigue, and difficulty concentrating. It takes one simple blood test to get your levels tested. A 25-hydoxy vitamin D test can tell your doctor if your vitamin D level is deficient or if you are at risk due to lower levels.
The 25-hydoxy test measures vitamin D levels in blood as nanograms per milliliter (ng/mL). Normal levels of vitamin D are between 30-40 ng/mL. Deficiency is a level less than 20 ng/mL, while toxic levels are anything greater than 150 ng/mL.
When vitamin D levels are normal, RA symptoms and pain and overall health are improved. The National Institutes of Health recommends a dietary allowance of 600 international units (IUs) per day of vitamin D. People who are deficient need more and may benefit from taking 1-2,000 IUs per day.
Patients who have been diagnosed with severe deficiency, or who have certain health conditions, may take a 50,000 IUs prescribed dose, over a longer period of time, i.e., twice a week. Too much vitamin D can cause toxicity, resulting in serious health issues.
According to the Vitamin D Council, patients are most likely to develop toxicity if they take more than 40,000 international units of vitamin D everyday for more than three months. Talk to your doctor before taking any high doses of vitamin D.
The sun is your best source for vitamin D but you shouldn’t sit in the sun for longer than 30 minutes per day without adequate protection, such as sun creams and screens. You can also acquire vitamin D from the foods you eat. Fatty fish, such as salmon and tuna, fish liver oils, vitamin D fortified milk and eggs are good vitamin D sources.