Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
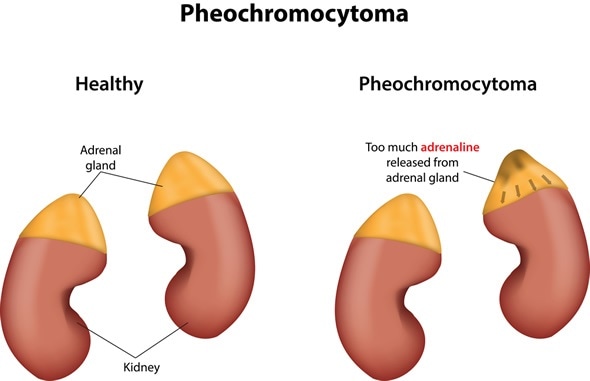
Pheochromocytoma is a term used to refer to rare and mostly benign catecholamine-secreting tumors arising from the chromaffin cells found in the adrenal medulla or in the paraganglia (i.e. extra-adrenal pheochromocytoma). Clinical presentation can be highly variable and can mimic other diseases, but the condition typically presents with hypertension, palpitations, severe headaches, and sweating.
As an entity, pheochromocytoma was initially described in 1886 by Frankel, following the autopsy of an 18-year-old that girl died suddenly in collapse, while the first successful surgical removal of the tumor was described in 1926 by Roux. Its name was established in 1912 by Pick and derived from Greek words “phaios” (meaning dusky), “chroma” (meaning color), and “cytoma” (meaning tumor).
The prevalence of pheochromocytoma in the general population is uncertain, although it is known that this condition accounts for less than 0.2% of patients with hypertension or high blood pressure. In approximately 10% of patients, pheochromocytoma is discovered incidentally during computed tomography (CT) or magnetic resonance imaging (MRI) of the abdomen for unrelated symptoms.
One study in Minnesota has shown that pheochromocytoma occurs in approximately 1-2 individuals per 100,000 adults every year. This suggests that if 20% of the adult population has high blood pressure, five pheochromocytomas would be expected among 100,000 hypertensive patients.
In a large series of patients that were screened biochemically for suspected pheochromocytoma, the incidence has been noted as high as 1.9% (occurring equally in women and men). In a study, one pheochromocytoma per 2301 autopsies was found. Unfortunately, the Mayo Clinic experience shows that in up to 50% of cases of pheochromocytoma the correct diagnosis is made at autopsy.
The condition occurs in people of all races (albeit they are less frequently seen in African Americans). Even though pheochromocytoma may occur at any age, the peak incidence is observed between the third and the fifth decade of life, with 10% of them occurring in children.
Pheochromocytoma usually occur as sporadic tumors, hence about 90% of them are presenting as unicentric and unilateral single adenomas. The remaining 10% of them are inherited, usually as bilateral and multiple, sometimes also found extra-adrenal (with similar histopathological traits).
Nevertheless, more than half of apparently sporadic pheochromocytomas found in patients with 18 years of age or younger are a result of an isolated identifiable mutation in germline DNA; this percentage can reach as high as 70% in children younger than 10. Thus, guided genetic testing and genetic counseling is imperative for children presenting with pheochromocytoma, regardless of the family history.
Inherited pheochromocytomas may be isolated (inherited as an autosomal dominant trait) or a component of hereditary tumor syndromes – primarily multiple endocrine neoplasia (MEN) 2A and 2B and von Hippel-Lindau (VHL) disease, the familial paraganglioma syndromes and, in rare instances, MEN 1, neurofibromatosis (NF) type 1 and the tuberous sclerosis complex.
Many of the aforementioned syndromes are autosomal dominant in nature, resulting in a 50% chance that the children of affected individuals will develop the disease. Therefore, genetic counseling and expert genetic testing should be offered to family members of the affected patient.