Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
The popularity of personalized medicine is dramatically increasing, improving the efficiency of treatments and the prognosis of patients.
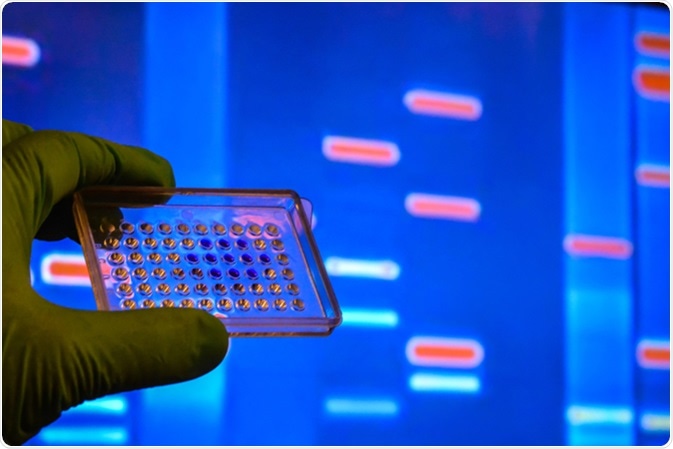
Each patient is unique, and therefore the “one size fits all” approach typically used within healthcare is not always effective. Therefore, personalized medicine utilizes genetic analysis to guide and improve medical practices, making treatments, diagnosis and prevention highly specific to each patient.
There are many uses of personalized medicine within healthcare. For example, patients which are unresponsive to traditional treatments can be prescribed more specific and effective drugs. Additionally, through the creation of susceptibility profiles, possible future diseases can be identified, which allows preventative action. Personalized medicine also helps diagnose patients in a highly specific manner, allowing more effective and targeted therapy.
However, despite the many advantages of personalized medicine, there are numerous issues which have started to arise, including ethical, legal and social problems. This article aims to highlight some of the most important issues that the industry will need to face before personalized medicine becomes more popular.
Intellectual property rights ensure that the individual who first has an idea has the exclusive right to develop it, this includes copyrights, patents and trademarks. However, with the development of genetic technology, these rights will have to be reassessed. For example, some argue that patenting DNA sequences may have a negative influence upon research and slow down the overall development process.
Additionally, another issue which needs to be reassessed are the regulatory frameworks. These are required to ensure that the standard of genetic testing and research is maintained at a high and reliable standard, however the current frameworks cannot be applied to personalized medicine.
A major issue within the field of personalized medicine is the ethics surrounding patient information.
Firstly, there are many ethical concerns relating to incidental disease discovery. Whilst a patient is being screened for one disease, the presence of another life-changing disease may be identified. This is particularly an issue if there are no available treatment options, as the prognosis of the patient is not improved during this process. Discovering that you have a disease can also have a very serious psychological impact on patients, leading to further ethical issues.
A secondary issue is the occurrence of false-positives, which occur when genetic factors are interpreted incorrectly and a patient is found to have a condition that they actually do not. This can lead to a plethora of both ethical and medical issues. These include, not only negative psychological effects, but also the application of inappropriate treatments, which can have a damaging effect on the patient and an unrequired expense upon healthcare.
The next issue is the rights of related family members. As genetic diseases are heritable and early intervention may prevent the development of the condition, some argue that the family should be informed if they are at risk. However, currently it would be the patient’s choice whether to tell their family or not.
Another issue which must be confronted is the stigmatization of individuals with certain diseases. If patient’s genetic data was leaked, many issues may be presented. For example, inappropriate use of this information by insurance companies, who may not offer policies to certain individuals with genetic diseases. Additionally, this information may also be used by employers, who may not employ someone based upon their genetic disease. This therefore highlights the importance of the security and confidentiality of genetic information.
Another issue is the increased requirement of genetic counselling. In order to make sure that patients are fully aware of their options and the significance of their genetic results, counselling will be required. Education of other staff members will also be required, ensuring that they understand the genetic tests which are available. Overall, scientists within the research labs need to work with doctors, and genetic counsellors to ensure that the patients receive the best possible care and advice.