Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
Periodontitis and diabetes are closely linked, and people who have poorly controlled diabetes are more likely to be affected by periodontitis.
This increased risk is primarily linked to the blood glucose levels. When individuals have a high level of glucose in the blood, an infection of the gums is more likely and the symptoms of the condition are often more severe. Additionally, pathological changes to the blood vessels that can occur in diabetic people can also increase their risk of being affected.
There are several reasons that people with diabetes are more likely to suffer from periodontitis, such as changes to the blood vessels.
Uncontrolled diabetes can cause thickening of blood vessels in the body, which may contribute to the increased risk of periodontitis. Blood vessels are responsible for the removal of waste products and delivery of nutrients all around the body, including dental structures. Thickening of the blood vessel walls can slow down the delivery of nutrients and removal of waste products, thus causing the body’s defenses against infection to become weaker.
Many types of bacteria thrive in the presence of sugars such as glucose. People with poorly controlled diabetes have higher levels of glucose in their blood than usual, which can provide the perfect environment for bacteria to proliferate in the mouth and eventually lead to periodontitis. It is for this reason that high blood glucose levels in diabetic can be problematic for dental health.
Fortunately, with adequate treatment and preventative techniques it is possible for people with diabetes to reduce the risk of being affected by periodontitis.
The first step is to ensure that the blood sugar levels are well controlled with adequate medications. Patients should be encouraged to speak to their doctor about their diabetes management plan to ensure that their condition is being controlled as well as possible. This plan typically includes frequent tests to check the levels of glucose of the blood so that the medication regimen can be altered as needed.
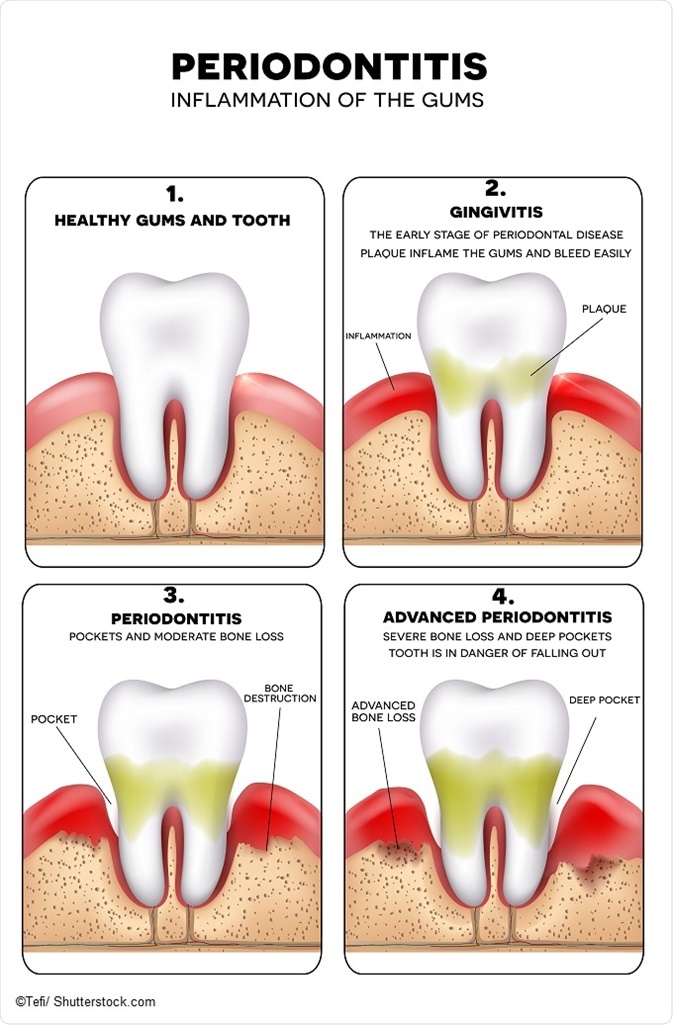
Additionally, it is important that patients follow general guidelines to protect their teeth and gums from gingivitis and periodontitis with regular teeth brushing and flossing. This is even more important for people with diabetes than for the general population because they are at an increased risk of the condition.
People with diabetes should also make sure that their dentists are aware that they have diabetes so that their care can be tailored and proper dental recommendations made accordingly.
It may be necessary for some changes to be made to the medical management of diabetes for patients with planned oral surgery.
Often, simple changes to the timing and doses of insulin are all that is required. However, in some cases for patients whose blood glucose levels are not well-controlled, it may be necessary to postpone dental procedures that are not urgent. Emergency procedures for acute infections should nonetheless be carried out immediately, with extra precautions being taken in the aftercare of the surgery.
It is also preferable for patients to retain their natural teeth by keeping the mouth and gums healthy because dentures and other replacements can contribute to problems. Ill-fitting dentures may cause pressure upon the gums and may cause discomfort, besides increasing the risk of periodontitis.