Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
 By Keynote ContributorDr. Amaal StarlingAssistant Professor of Neurology,
By Keynote ContributorDr. Amaal StarlingAssistant Professor of Neurology,Migraine, a neurologic disease that affects more than 38 million Americans of all ages, is often misunderstood and misdiagnosed by patients and physicians alike.[i],[ii] On the other hand, 24 million Americans of all ages have asthma and even those unaffected would most likely be able to recognize its symptoms, signs, and associated disability.[iii]

Woman having a migraine headache; Credit: kurhan / Shutterstock.com
The disparity of how both are viewed and therefore, treated, is telling. As strange as it may seem, migraine should be treated similar to asthma. No, really, it should. Think about it. Both diseases present symptoms in need of immediate rescue, and both conditions aim to achieve the ultimate goal of disease prevention.
For those with asthma, the road to diagnosis and treatment is typically more straightforward and without associated stigma. And, it’s high time that those living with migraine are entitled to a level of awareness and treatment protocols that work for them.[iv],[v]
To be clear and obvious, asthma and migraine are not related as one is a respiratory condition and one is a neurological disease. However, both are complex, chronic diseases with diverse triggers and symptoms that can be debilitating and impact overall quality of life.[vi],[vii],[viii],[ix]
Migraine is a neurologic disease that is characterized by recurrent, severe attacks of head pain and other associated symptoms. Along with head pain, migraine symptoms typically include nausea and vomiting, extreme sensitivity to light and sound, and some may experience disturbances in vision, sensation, or speech.[x]
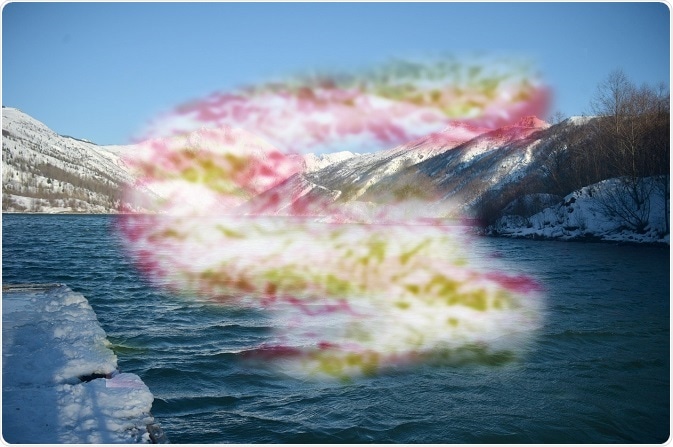
Visualization of visual disturbances experienced during a migraine. Credit: Jonathan Lingel / Shutterstock.com
It is often misunderstood by people with migraine who may assume “it’s just a headache” that they have to deal with on their own. In fact, only one out of three people who experience a migraine attack actually talk to their doctor about their symptoms and only half of those individuals are diagnosed properly.[xi]
Most often, migraine is misdiagnosed by doctors as tension-type headaches or sinusitis, and as a result, some patients are not provided with the appropriate treatment plan to see relief.[xii] That is a double whammy as not only is the attack left untreated, but the pain of a migraine attack can be severe and cause significant pain for hours to days, leaving people with migraine unable to work or function in day-to-day living.[xiii],[xiv]
Generally, the treatment of asthma has an understood approach to disease management. Most people with asthma need two kinds of therapy: quick-relief medicines to rescue them from short term symptom escalation (e.g., wheezing attacks) and long-term control treatments to reduce asthma attacks and control the disease day-to-day.
Patients are typically instructed to take long-term control medicines every day, even if they don’t have symptoms, to reduce airway inflammation; keep asthma under control regularly and to help prevent future asthma attacks.
Additionally, quick-relief medicines such as short-acting beta agonists/bronchodilators and oral corticosteroids are given to patients to help provide relief from the immediate asthma symptoms. Essentially, these treatments help ease relax airways, making it easier to breathe during an asthma attack. They do not, however, control the airway inflammation that causes the attack.[xv], [xvi]
All in all, people living with asthma are given a plan of action. But why isn’t it the same for those with migraine? Similar to those with asthma, people living with debilitating migraine can benefit from rescue medication when suffering an attack followed by true preventative care.[xvii]
Currently, the focus for migraine treatment tends to stay on rescuing the patient from acute attacks quickly and without significant adverse events to ensure they can continue with daily functioning.[xviii]
While prevention should be the ultimate goal, providing preventative care appropriately for those with migraine can be difficult. Patients are candidates for preventative treatment IF:
Overall, preventative management, from lifestyle changes to available medications, is underutilized for treating migraine.[xix] Preventive options are trialed in a step-wise fashion. In some cases, patients find that their health insurance prevents immediate access to recommended treatments.[xx]
For example, a patient may be instructed to try (and fail) a different, less expensive treatment (rescue or preventative) before being able to try a more expensive or potentially new option.[xxi]
Lifestyle changes such as good sleep hygiene, eating regular, healthy meals, exercising weekly, drinking water and fluids, relaxation and stress management techniques, and eliminating food triggers are some ways to help prevent a potential migraine attack.
In my experience, these approaches aren’t discussed enough, but they should be because they can be integrated into a treatment plan without costing the patients a dime or resulting in side effects.
Further, encouraging patients to track their symptoms on a daily or weekly basis using a headache diary can help gauge what part(s) of their plan may or may not be working.[xxii]Part of a successful treatment plan relies on putting the patient in the driver’s seat to manage their condition.
Currently available treatment options are not disease-specific, mechanism-based, targeted treatments; thus, they lack consistent efficacy and often cause side effects. The majority of patients discontinue preventive treatment options due to inefficacy and side effects.
However, there is potentially good news on the preventive medication front for both patients and physicians. All sides are keeping a close eye on late stage research surrounding a new class of investigational treatments referred to as anti-CGRPs or calcitonin gene-related peptide (CGRP) inhibitors.
These investigational medications would be the first therapies specifically designed to treat migraine. Findings from Phase 3 trials give reason for excitement as these potential treatments may provide options that are better tolerated and with no reported safety issues.[xxiii]
It should be noted that if approved, patients can expect these treatments to be more expensive than currently available medications with or without insurance. Patients can stay up to date on issues on migraines at the 50 State Network. The idea that migraine finally has focus for prevention is encouraging for millions.
All in all, there needs to be greater acceptance that migraine is a complex neurological disease in need of better management. Providers (and their patients) need increased education about migraine, its associated disability, and the treatment options that may best suit individuals based on their attack frequency, treatment goals, and medical history.
It’s time to treat one of the most disabling disease in the world, migraine. We must establish pathways to resolution that are concrete and eventually commonplace, as they are for those with asthma.
It’s simply time to treat migraine.

Assistant Professor of Neurology
Mayo Clinic
Scottsdale
Arizona, USA
Dr. Starling is an Assistant Professor of Neurology in the Mayo Clinic College of Medicine. She joined Mayo in 2012 and is currently a Consultant within the Department of Neurology.
Dr. Starling received her M.D. degree from the Drexel University College of Medicine in Philadelphia, and completed her Neurology Residency and a Headache Fellowship at the Mayo Clinic College of Medicine in Scottsdale, Arizona.
She serves as a member of the AHS Annual Meeting Scientific Committee. Dr. Starling has been the recipient of numerous awards including the AHS Above and Beyond Award for Service, and the Manfred D. Muenter Award for Excellence in Clinical Neurology.
Dr. Starling’s main fields of interest include migraine, concussion, posttraumatic headache, trigeminal autonomic cephalalgias, secondary headaches, telemedicine and teleconcussion, and neurology resident education.
[i] Migraine Research Foundation. Migraine Facts. Available here: http://migraineresearchfoundation.org/about-migraine/migraine-facts/. Accessed February 16, 2018.
[ii] Al-Hashel, J, Ahmed, SF, et al. Migraine misdiagnosis as a sinusitis, a delay that can last for many years. Journal of Headache Pain. 2013 Dec; 14(1): 97.
[iii] The Centers for Disease Control and Prevention. Asthma. Available here: https://www.cdc.gov/nchs/fastats/asthma.htm. Accessed February 16, 2018.
[iv] Mayo Clinic. Asthma Attack Overview. Available here: https://www.mayoclinic.org/diseases-conditions/asthma-attack/symptoms-causes/syc-20354268. Accessed February 16, 2018.
[v] Mayo Clinic. Migraine Overview. Available here: https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201. Accessed February 16, 2018.
[vi] Mayo Clinic. Asthma Attack Overview. Available here: https://www.mayoclinic.org/diseases-conditions/asthma-attack/symptoms-causes/syc-20354268. Accessed February 16, 2018.
[vii] Mayo Clinic. Migraine Overview. Available here: https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201. Accessed February 16, 2018.
[viii] Medication non-adherence and asthma treatment cost; BG Bender, C Rand; Curr Opin Allergy Clin Immunol, 4: 191-195, 2004.
[ix] American Migraine Foundation. Living with Migraine. Available here: https://americanmigrainefoundation.org/living-with-migraines/. Accessed February 16, 2018.
[x] Mayo Clinic. Migraine Overview. Available here: https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201. Accessed February 16, 2018.
[xi] American Migraine Foundation. Living with Migraine. Available here: https://americanmigrainefoundation.org/living-with-migraines/. Accessed February 16, 2018.
[xii] Al-Hashel, J, Ahmed, SF, et al. Migraine misdiagnosis as a sinusitis, a delay that can last for many years. Journal of Headache Pain. 2013 Dec; 14(1): 97.
[xiii] Mayo Clinic. Migraine Overview. Available here: https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201. Accessed February 16, 2018.
[xiv] American Migraine Foundation. Living with Migraine. Available here: https://americanmigrainefoundation.org/living-with-migraines/. Accessed February 16, 2018.
[xv] American College of Allergy, Asthma and Immunology. Asthma Treatment. Available here: http://acaai.org/asthma/asthma-treatment. Accessed February 16, 2018.
[xvi] Mayo Clinic. Asthma Diagnosis and Treatment. Available here: https://www.mayoclinic.org/diseases-conditions/asthma/diagnosis-treatment/drc-20369660. Accessed February 16, 2018.
[xvii] Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007;68:343-349.
[xviii] American Academy of Neurology. Migraine Headache Guidelines. Available here: https://www.aan.com/guidelines/home/getguidelinecontent/120. Accessed February 16, 2018.
[xix] Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007;68:343-349.
[xx] Cottrell, C, Drew, J, et al. Perceptions and needs of patients with migraine. J Fam Pract. 2002 Feb; 51(2): 142-147.
[xxi] Cottrell, C, Drew, J, et al. Perceptions and needs of patients with migraine. J Fam Pract. 2002 Feb; 51(2): 142-147.
[xxii] Mayo Clinic. Migraine Diagnosis and Treatment. Available here: https://www.mayoclinic.org/diseases-conditions/migraine-headache/diagnosis-treatment/drc-20360207. Accessed February 6, 2018.
[xxiii] Tso, A, Goadsby, P. Anti-CGRP monoclonal antibodies: the next era of migraine prevention. Curr Treat Options Neurol. 2017 June; 19(8): 27.