Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
Neurogenic bladder control is a condition of loss of urinary function due to nerve, spinal cord or brain damage. A variety of circumstances can lead to neurogenic bladder, including spinal injury, neurologic disorders, or systemic disease of the body like diabetes.
Neurogenic bladder can manifest as an overactive bladder, with leakage and poor control. It can also appear in the form of an underactive bladder that does not empty properly when full. Once the diagnosis is complete, management of overactive bladder usually entails several strategies.
In the case of partial or complete urinary retention, clean intermittent catheterization (CIC) is a common method of management. The technique is appropriate if the patient or their caregiver has sufficient coordination to perform the procedure.
However, it is not workable for patients who cannot perform it and without a caregiver who can. It is also not a good option for patients who present with the abnormalities of the urethra or poor cognition. CIC is usually performed every 4-6 hours to keep the bladder from becoming overdistended.
An indwelling catheter is sometimes used when CIC is not feasible. It carries an increased risk of renal failure, bladder stones, renal stones, urethral fistulas, strictures, urethral erosion, and bladder cancer. An option for patients with incomplete injury with some bladder control remaining is timed voiding.
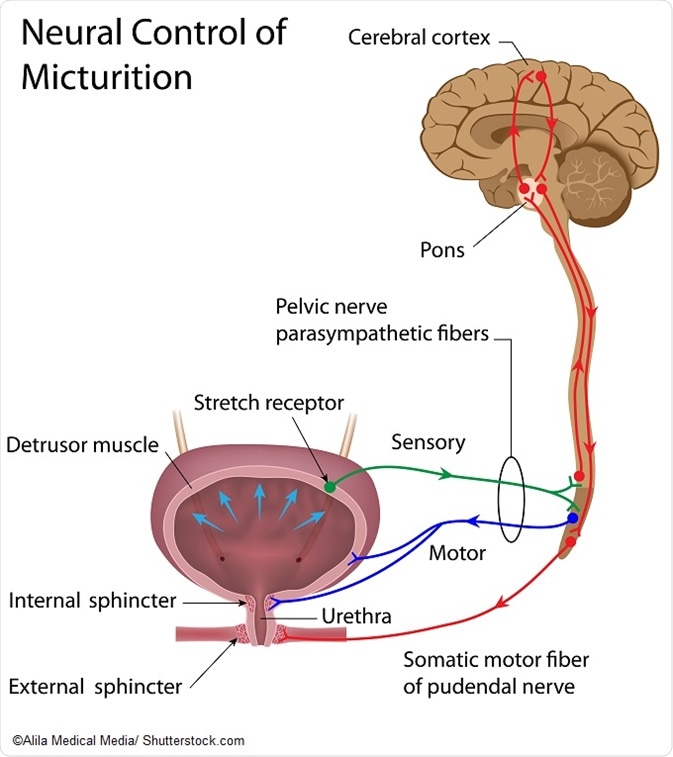
Antimuscarinics represent a first-line option in managing neurogenic detrusor overactivity (NDO). Contractions of the detrusor muscle are mediated by the M2 and M3 muscarinic receptors. Anti-muscarinic agents stabilize the detrusor muscle, making it more responsive to signals from the parasympathetic nervous system. However, high doses are required in these patients, and the high rate of severe side effects lead to poor tolerance of the therapy.
A class of drugs known as beta-3 adrenoreceptor agonists have come into use for overactive bladder. These drugs reduce the number of times the bladder is voided per 24 hours, improving in turn other symptoms and quality of life.
Injections of the toxin from the bacterium Clostridium botulinum are now in use for NDO in patients who have failed other medical therapy. The alternative for these patients previously was indwelling catheterization, diapers, or even major reconstructive surgery.
A number of surgical options are available for neurogenic bladder. These include:
Intravesical vanilloids have been used to treat neurogenic bladder caused by detrusor overactivity. These agents activate TRPV1, which results in membrane depolarization and release of sensory neuropeptides.
A meta-analysis of literature on the use of one of these compounds showed symptomatic and urodynamic improvement in 84% of patients with neurogenic detrusor overactivity (NDO). Combining the compound with another to improve tolerability resulted in enduring benefits. TRPV1 is of continued interest as a target for NDO and a number of other disease indications.
Patients with neurogenic bladder due to spinal injury require surveillance. A typical annual surveillance appointment includes a history, physical exam, and laboratory tests. Urodynamic screening can be carried out at intervals of around 5 to 10 years.
Also, it must be noted that neurogenic bladder increases the risk of bladder cancer development. Rates of bladder cancer among patients diagnosed in their 40s and 50s range from 0.27% to 10%. Factors such as inflammation, irritation, infections, stones, and indwelling catheters contribute to the risk.