Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
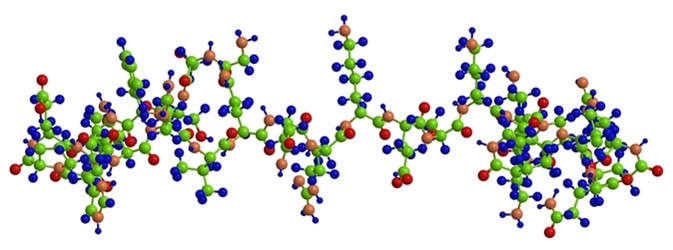
Leptin and ghrelin are two key peptide hormones which regulate energy metabolism via appetite modulation. They also play a vital role in regulating body mass in response to sleep duration as well.
Ghrelin is an orexigenic hormone, but increasing the appetite is not the only function it has. Instead, this hormone has many metabolic and anabolic effects in various parts of the human body.
A plethora of different environmental factors have been studied in the genesis of obesity (i.e. a condition where a person accumulates an excessive amount of body fat), which includes the Circadian clock, eating patterns, and sleep reduction.
In most industrialized countries, the daily sleep duration has gone down by an hour and a half. This is temporally linked to a steep rise in the incidence of obesity, and has given credence to the hypothesis that sleep disruption can modify the biological rhythms of feeding behavior, which in turn leads to weight gain and obesity.
Many workers report that when the average duration of daily sleep is less than 7.7 hours, individuals of all age groups show a higher mean BMI, as well as leptin reductions and ghrelin increases that are independent of age and sex. These hormonal changes are as akin to those which occur with poor energy intake or weight loss, and lead to increased eating. This is a biologically plausible mechanism for the increased BMI that accompanies poor sleep.
Ghrelin acts on the hypothalamic-pituitary axis and other areas of the brain to stimulate a feeling of hunger and promote feeding. When a person sleeps, leptin levels normally rise, subduing the need to eat by reassuring the brain that energy reserves are adequate for the time.
However, sleep deprivation increases ghrelin levels, while at the same time lowers leptin levels in the blood. The latter phenomenon is a signal of a limited energy supply to the brain. Subsequently, the message sent out to the gastrointestinal tract is one of hunger, and as a result the person starts to eat (though there is no real need to).
Ghrelin levels rise primarily in response to acute sleep deprivation, while leptin levels fall with chronic sleeplessness. A single night of poor sleep causes acute rises in ghrelin levels, but leptin concentrations remain essentially the same. The mechanism is via neuropeptide Y (NPY) and agouti-related peptide (AgRP), leading to suppression of neurons which secrete proopiomelanocortin or cocaine/amphetamine regulated transcript neurons.
These put forth a positive signal which stimulates feeding. In short, this means that a single night of sleep loss profoundly disrupts normal energy homeostasis, causing a high risk of obesity.
Thus both metabolism and neuronal mechanisms underlie feeding and sleep patterns. An example is the occurrence of feelings of hunger during the daytime simultaneously with maximum alertness, but feelings of fullness and sleepiness once darkness sets in.
The effects of chronic sleep deprivation are many, and range from tiredness in the morning hours to mental slowness and prolonged feelings of tiredness. The final result is reluctance to engage in physical work or exercise.
A preference for the evening hours sets in, more frequent in certain alleles coding for some circadian rhythms. Ghrelin increases non-rapid eye movement (NREM) sleep probably via the growth hormone–releasing hormone (GHRH) receptor. This knowledge has the potential to help in formulating sleep aids which are more tuned to normal physiology.