Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
An epidermal nevus is an overgrowth of one of the cell species found in the epidermal layers and appendages. In many patients, an epidermal nevus syndrome (ENS) is present. This is marked by the presence of not only epidermal nevi but other defects of the brain, eye, and bones. However, the combination of hypophosphatemic rickets with epidermal nevi is very uncommon, occurring mainly in Schimmelpenning syndrome or SFM syndrome.
Schimmelpenning syndrome is a condition in which there are multiple sebaceous nevi, along with skeletal or neurologic manifestations, and is the most common type of ENS. Usually presenting in childhood or puberty, the lesions are present at birth, and consist of smooth hairless yellowish-red patches, commonly on the scalp and mid-face, though the extremities may also be affected. They thicken and become rough over time.
In this condition, some patients have a large epidermal nevus-affected area, often covering one side only. It is accompanied by tumors of the bone, lungs, and the skin. The bones form cysts or may fracture easily. This leads to progressive bone pain, deformity, and loss of stature. The low phosphate levels and vitamin D deficiency can cause hypophosphatemic rickets.
Rickets in ENS is thought to be due to some factor present in the epidermal nevi. This is another form of the osteomalacia often present in tumors, termed oncogenic osteomalacia, whereby certain benign tumors both in and outside the bone lead to renal wasting of phosphorus, causing hypophosphatemia, but reduced secretion of plasma calcitriol. These are the identical metabolic defects found in this ENS. Excision of the epidermal nevi, just like the removal of the tumor, leads to correction of the symptoms such as bone pain. The most common tumors that cause this type of rickets are ossifying fibroma-like tumors and osteoblastoma-like tumors.
The presence of phosphatonin-like substances in epidermal nevi is suspected by the fact that injecting material from the nevi in an ENS patient led to phosphaturia in the recipient. The level of FGF-23 was found to be raised in one of these hypophosphatemic ENS patients. The excision of the lesions brought about significant correction of bone mineralization and bone pains.
Hypophosphatemic rickets in ENS presents with growth failure, bending of bones and deformities, bone pain, limping or inability to walk, chest deformities and multiple fractures. Bone cysts often occur in ENS. In some cases, central nervous defects such as mental retardation is also present.
Individuals affected by Schimmelpenning syndrome have defects of the central nervous system, leading to mental retardation and even malformations such as arachnoid cysts.
Ocular anomalies include the occurrence of colobomas, retinal defects, corneal opacities, optic nerve defects, and strabismus. Lipodermoids are also reported in this syndrome, as fatty tumors on the outer part of the eyeball.
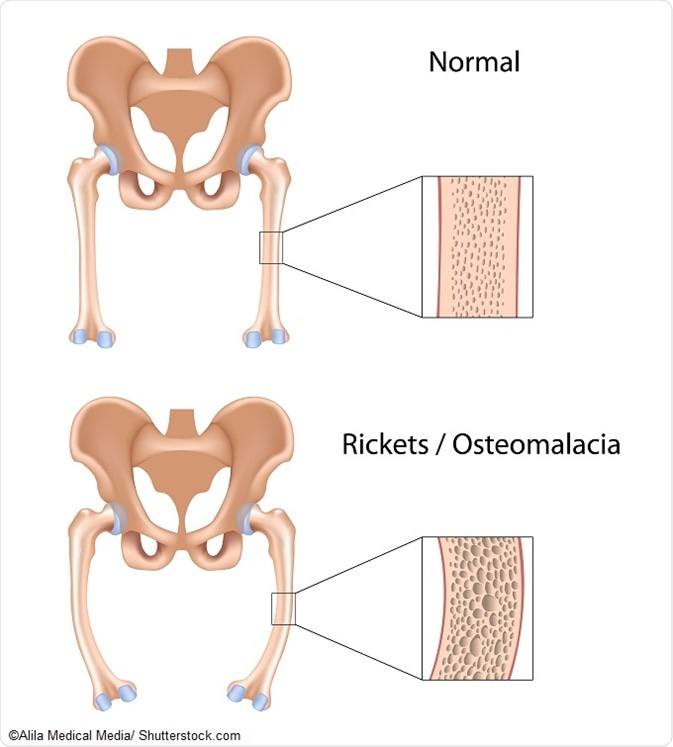
Skeletal abnormalities include typical manifestations of rickets, frontal bossing, and bone cysts. Several parts of the skeleton may be underdeveloped. Vitamin-D resistant rickets is also present.
The calcium and phosphorus levels in serum are low, while the serum alkaline phosphatase is high, indicating failure of bone mineralization and increased bone resorption. The parathyroid hormone level is also higher than normal.
Phosphaturia is present, but other serum tests are usually normal.
Radiology reveals the typical features of rickets with osteopenia, flaring, fraying and cupping of the metaphyses, with scoliosis of the thorax and lumbar spine. There are multiple fractures of the femurs and ribs.
Treatment is usually with alfacalcidol or calcitriol along with acidic phosphate solution. This usually leads to clinical and radiological improvement, with healing at the metaphyseal ends and relief of bone pain. Serum levels of phosphorus and alkaline phosphatase remained low and high, respectively, throughout treatment, despite obvious success in alleviating the symptoms. Excision of the lesions led to improvement in serum parameters as well to near normal levels.