Site Under Development, Content Population and SEO, Soft Launch 1st January 2020
Colorectal surgery is a medical operation that is performed on the colon, rectum and anus. Colorectal surgeons, who are also referred to as proctologists, are responsible for carrying out this procedure, which may be necessary to treat a number of conditions.
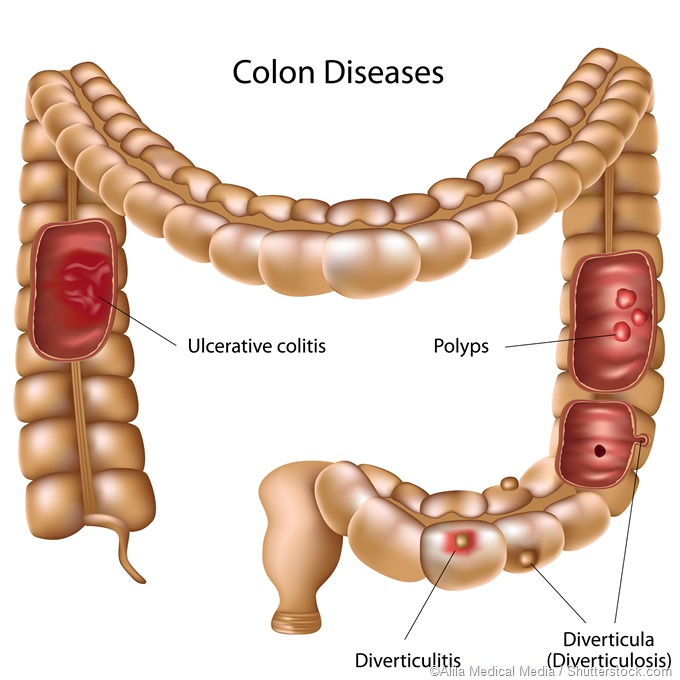
These problems can be acquired or congenital, and include, but are not limited to, Crohn’s disease, ulcerative colitis and neoplastic lesions in the colorectal region, as well as birth defects (such as imperforate anus), fissures, fistulas, hemorrhoids, rectal or anal prolapse, fecal incontinence, diverticulitis, diverticular disease and other disorders.
Colorectal surgery may employ many different techniques, such as colectomy, stricture-plasty, lateral internal sphincterotomy, ligation, transanal endoscopic microsurgery, anoplasty, bowel diversion, colostomy and polypectomy. Colectomy may involve resection of the entire colon with the rectum, or only a part of it.
Lateral internal sphincterotomy is a procedure performed to treat tears or anal fissures, whereas bowel diversion surgery is necessary to reroute the passage of stools from the body, following removal of part of the bowel has been removed, or in order to give the injured bowel time to heal.
Transanal endoscopic microsurgery is minimally invasive surgery aimed at the removal of large rectal polyps. It is an alternative to other traditional transanal techniques and rectal resection, and it is associated with low rates of recurrence. This is because the technique allows excellent visualization of the surgical area and thus increases the precision of the dissection.
Anoplasty refers to the surgical reconstruction of the anus in order to treat conditions such as imperforate anus. Colostomy is usually performed after bowel resection or trauma, to create an opening for the bowel emerging through the abdominal wall. This is necessary to provide an exit point for stool, which may be temporary or permanent. Polypectomies are required for the removal of polyps that have malignant potential.
The most common contemporary approach to colorectal surgery is laparoscopic, which uses an internal camera and specialized surgical tools. This approach avoids the need for creating long incisions on the abdomen, thereby reducing post-operative pain and speeding up the recovery process.
Carbon dioxide is used to inflate the abdomen and a few very small incisions are needed. It is through these incisions, viewing the interior of the abdomen on a video monitor, that the surgeon performs the necessary operation. In earlier times, laparoscopy was mostly done for gynecological and gallbladder surgeries, but is now widely used today for colorectal procedures.
Post-surgical complications vary in incidence and severity, depending on the indication for surgery and the type of procedure done. They include excessive bleeding, such as may occur after traditional or open colorectal surgeries or intestinal perforation, and damage to the reproductive and genitourinary organs and structures.
Patients may develop serious infections within the abdominal cavity after the surgery. Some patients may have negative responses to the anesthetics used, and in others, there may be scarring, which may cause emotional or occupational distress to the patient. The risk of complications increases with increasing age of the patient.